When Joseph B. Martin relinquishes the deanship of Harvard Medical School (HMS) at the end of the academic yeara decision announced on October 5he will have put in place a new curriculum and the enormous New Research Building: tangible evidence of the schools teaching and scientific missions. But much behind-the-scenes workreconstructing the relationship between HMS and its affiliated hospitals, planning for the conduct of basic science and clinical activityunderlay those advances, and will continue to shape Harvards extensive biomedical work in the next decade.
During a mid-November conversation reviewing his service as dean since 1997, Martin focused first on the revamped curriculum, a new approach driven by the changes in the healthcare system. The hospitals pursuit of high-occupancy, high-throughput medicine has made it much harder for students to get the extended exposure to patients that they need to gain proficiency. By shifting from a series of rotations among as many as seven institutions to immersion in one during their third, clinical year of medical study, students gain opportunities to follow patients in depth, understand the organizational context of medicine, and develop relationships with their mentors (see The Pulse of a New Medical Curriculum, September-October 2006, page 64, for a detailed report). Reaction has been appreciative and enthusiastic, Martin said. Meanwhile, the first two years of classwork have been improved by bringing faculty members together to integrate the content so that learning progresses from course to course.
Effecting this kind of change is especially difficult because HMS depends on the hospitals for most of its teaching faculty: their appointments are contingent on a minimum of 50 hours of teaching annually. Early in his tenure, when some of the hospitals were under acute financial pressure, Martin arranged to boost payments to the hospital-based faculty members who hold endowed chairs, assuring that education would remain a priority. In the current environment, he disclosed, HMS and the hospitals have jointly agreed to boost their spending on hourly stipends for other clinical faculty members who agree to teach more than the annual minimum. The new fundsa 40 percent increase, bringing such spending to $15 million annuallyhelp encourage the hospital-based faculty to balance patient care and teaching.
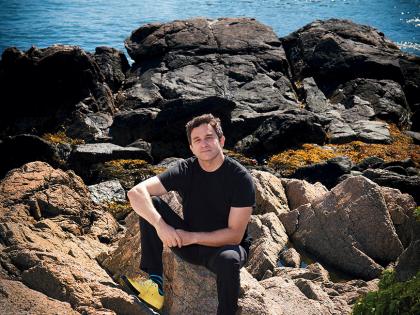
|
|
| Joseph B. Martin |
| Photograph by Graham Ramsey / Harvard Medical School |
This small example points to a much larger theme in Martins deanship. Relationships with the hospitals, he said, now are characterized by thoughtful, open, transparent discussions around the academic mission. Thats a radical change from the situation in the mid 1990s, when Bostons major teaching hospitals formed partnerships, consolidated staffs, and courted one anothers star doctors in an aggressive effort to bring in patient and research revenue.
I thought healing of those relationships for mutual advantage was the most important thing I could do at the beginning of his tenure, Martin said. Having been based at Massachusetts General Hospital (MGH) earlier in his career (Martin is Walker professor of neurobiology and clinical neuroscience), he brought affiliate and HMS perspectives together at a time of quite ugly competitions. He was particularly disturbed, for instance, by the financially stronger institutions poaching of staff from weaker hospitals, a practice that needed to be refereed. It now is, by a council of academic deans who agreed to standards for such lateral recruitment across their institutions, review them, and discourage community-degrading hirings that are not legitimate promotions, Martin said.
More broadly, as dean, he began monthly, individual meetings with the hospital CEOs, in their offices or his own. Given the distance across Boston to MGH, Martin holds office hours there at least eight days a year. From such contacts have come cooperative searches for new faculty, joint research strategies, and, in spirit at least, shared governance. There are now cooperative centers, involving hundreds of researchers at HMS and the affiliates, that address cancer, neurological disorders and injuries, and other critical biomedical problems. Martin also became personally involved (with the institutions trustees) in searches for new leaders of Dana-Farber Cancer Institute, Beth Israel Deaconess Medical Center, and Childrens Hospital.
The strength of those ties will likely be tested anew. Three years of level research funding from the National Institutes of Health Research, after an extended period of vigorous growth, will create new tensions, Martin said. Each hospital plans further research expansion, and tight resources will heighten friction about retaining current faculty and researchers and recruiting new ones. In such circumstances, education is always in jeopardy of being reduced in its importance relative to the enormous research and clinical enterprises.
Fueled (until recently) by fundamental discoveries and the abundance of funds, the research itself is burgeoning, in fields from genomics and proteomics to clinical investigations across the spectrum of illnesses. In addition to creating a large systems biology department (see Seeing Biological Systems Whole, March-April 2005, page 67), the medical school has launched a raft of new programs to train future leaders in academic and institutional medicine, including: Ph.D. programs in systems biology and in chemical biology with the Faculty of Arts and Sciences (FAS); a joint M.D.-M.B.A. program with Harvard Business School; and a social-sciences track within the existing medical Ph.D. course of study.
Scanning the array of research initiatives, Martin said, The startling thing about biology, about how cells work and go wrong, is how complex the solutions will turn out to be. He noted that the Human Genome Project, assumed to get at the medical holy grail by identifying each human gene, had been completed before RNA interference was even discovered, in 1998; this fundamental mechanism, recognized last October with a Nobel Prize, has completely transformed how we think about genetics, suggesting that the means of switching genes on and off are even more important than the genes themselves. That implies whole new layers of research, investigations of abnormalities, searches for sites for medical intervention, and design and trial of therapies. For all the translation of knowledge into potential drugs, he said, Basic, fundamental research is where most of the rewards are going to come from. Given HMSs prowess as a research institution, We ought to protect that in every way possible, from junior faculty searches through support of graduate students to appointment of the scientists who lead the core departments.
To sustain such research at Harvard, Martin said, science planning in a way thats never been done before is really critical, especially during the next 10 yearsa priority also identified by President Derek Bok and FAS dean Jeremy R. Knowles (see Interim Agendas, November-December 2006, page 65). New techniques, equipment, and lines of inquiry are all advancing; with plans proceeding to build a science complex in Allston, new spaces in which to work on integrative science are near at hand. But the University, Martin cautioned, has much work to do to discern the ways to organize itself for such research effectively and efficiently. Allston ought to be thatthe physical and intellectual working out of ways as yet unperfected for collaborative science, productively disrupting current norms without violating useful disciplines and controls.
Alongside that basic research, Harvard also needs to envision a whole new way of approaching clinical investigation, in order to translate discoveries into medical applications. Acute-care hospitals do the work now, expensively, Martin said. In an era of genomic and proteomic science, when physicians may acquire detailed knowledge of an individuals genetics and hundreds of possible molecular targets for, say, a cancer treatment, a whole new paradigm for evaluation and testing may be required. Moving to create such a facility and processes, in Allston or alongside HMS (if the Harvard School of Public Health relocates to Allston), must be a priority for the next decade, he believes.
Whether the public keeps faith with biomedical progress, of course, depends on its trust in scientists. Martin has worked extensively to maintain standards that minimize financial conflicts of interest and promote full disclosure of funding sources, so that researchers are above reproach. That work was not universally popular at first, but has since been widely emulated within academic medicine (see Controlling Conflicts of Interest, September-October 2004, page 76). Last autumn, he again reminded HMS and affiliated researchers of their obligation to fully disclose all financial relationships when publishing in the leading medical journals; recent violations of that policy had prompted wide news coverage and professional criticism.
Waving off objections to HMSs strict policies, Martin said there was no evidence that they have discouraged research or the commercialization of promising discoveries. To the contrary, a paper he and a coauthor published in December explores different obstacles to productivity, at least in neurological drug discovery; they identify organizational barriers, including the ways in which intellectual property (read: marketable knowledge) is sequestered, rather than pushed ahead for patient use. Martin expects to explore this topic further during his forthcoming sabbatical year.
Leading the medical schoolwith its half-billion-dollar budget, its 1,500 students, and (counting the affiliated institutions) several thousand interns, residents, and postdocs, and its 7,000-plus faculty membersis perhaps the most complex decanal position at Harvard. Martin said generosity without a grudge had proved an effective style of managing and making decisions. His successor will need that and more. As for himself, Martin said, after a fulfilling decade at HMSs helm (and prior executive leadership at the University of California, San Francisco), he looks forward to resuming his professorial duties: I dont plan to run anything ever again.