The U.S. healthcare system is “Big, fat, and sick.” So said professor of medicine Jag Singh, speaking at a recent conference in Boston—where his efforts to champion innovations in digital healthcare took center stage. Singh, a former clinical director of cardiology at Mass General Hospital, underscored the urgent need for innovations in digital healthcare.
Healthcare expenditures account for about one-sixth of U.S. Gross Domestic Product—yet, outcomes remain poor, and many Americans are effectively excluded from care. Recent research on private-equity investment in medicine suggests a decline in the quality of care. Singh and others believe that the remedy to problems of cost, access, and quality lies applying digital technologies to the healthcare system.
This sentiment was echoed at the Mass Brigham General's Assembly Row campus during the public opening of Medically Engineered Solutions in Healthcare (MESH) Core 2024, a two-day intensive healthcare innovation bootcamp. Sponsored by Harvard Innovation Labs, MESH Core aims at empowering biomedical startup CEOs, practicing physicians, medical researchers, and investors to drive innovation in healthcare.
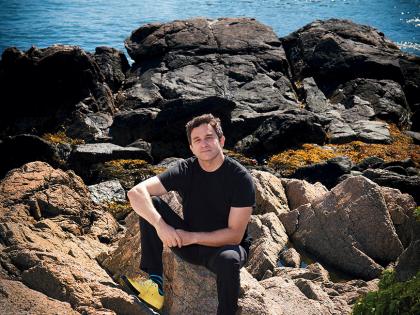
As a global hub for healthcare and life sciences, Boston provided an ideal backdrop for this endeavor. The program was spearheaded by assistant professor of radiology Marc D. Succi, founder and executive director of MESH, with the goal of equipping clinicians with the necessary skills to embrace new technologies, navigate patenting processes, and pursue other steps essential to effect healthcare innovation—from training doctors and optimizing the workflows in hospitals to empowering patients to access care.
Held from the 20th-21st of May, this "bootcamp" is an accelerated version of the same week-long course, offered on a rolling basis from Mass General Brigham Innovation. Its curriculum represents the first integrated innovation course in a hospital system, and an Accreditation Council for Graduate Medical Education (ACGME)-accredited medical training program. Over 290 attendees from 10 countries made it to the conference, which Succi hopes to make public again next year.
The Smartphone and Artificial Intelligence Revolution in Healthcare
Ninety percent of U.S. adults have smartphones. As Singh told conference attendees, he believes the medical smartphone revolution is the next frontier in digital health – with apps designed to deliver concierge-level services directly to patients via a virtual doctor (or real one), able to answer questions about symptoms and begin immediately determining a course of treatment. Realizing this vision, of course, involves overcoming multiple hurdles, from designing the care to satisfying regulatory requirements and reconfiguring reimbursement models to facilitate widespread adoption.
Singh also touched on the role of artificial intelligence (AI) in revolutionizing healthcare. AI solutions are already being employed to collect, aggregate, and organize vast amounts of data within health systems. These technologies hold promise in clinical decision-making, hospital management, and predictive analytics.
Generative AI models such as ChatGPT can be used to decode datasets, write computer programs, and summarize information, playing an assistive role in healthcare. Within hospitals, Singh said, these tools can also be adapted for clinical decision-making and predictions on whether discharged patients may require readmission—a key tool in tracking the trajectory of their health outcomes.
Before such applications become practicable, however, the application of AI to medicine itself must be improved. Large language models (LLMs) analyze vast amounts of data, but can misrepresent the variable demographic characteristics of patients. Artificial intelligence can be used to optimize healthcare processes, but practitioners and users need to be able to recognize potentially biased training sets. These and other pitfalls in AI application, Singh noted, will require reskilling current doctors, and training the physicians of the next generation, for our ecosystem of rapidly evolving technology.
MESH Core aims to help fill this gap by democratizing medical innovation education. As the program’s leader, Succi advocates for incorporating innovation competence into medical school and residency curricula, envisioning a future where healthcare professionals are better equipped to drive and embrace change.
This is the purpose of MESH Core: to be one of the first programs of its type that helps educate doctors on medical device development and digital health tools. “With MESH, we’re hoping conferences like this could start out a conversation about medical tech and innovation education requirements for doctors,” Succi told Harvard Magazine.
Succi hopes to encourage change in the governance of medical education, “requir[ing] all schools and all residencies to have a minimum competence of innovation in the people they graduate”—both to accelerate innovation, and to equip clinicians to adapt and deploy those innovations as they enter practice.
Other speakers from Harvard included Kate Coffman, associate professor Harvard Business School; Jorge Cortell-Albert, senior advisor, Healthcare and Life Sciences Harvard Innovation Laboratories; and Jeff Karp, professor of anesthesia, Harvard Medical School, who each offered their perspectives on the digital health transition in medicine and business.
“I think if we [make these requirements], in 10 or 15 or 20 years we’re going to see many practitioners who are better poised to make innovations,” Succi said. In the face of resumed cost inflation in healthcare, hospital capacity limits, and steadily rising wait times—atop the perennial problems of limited access and disappointing health outcomes relative to high U.S. expenditures—the MESH program is an example of how hospital systems can adapt to digital innovation as broadly and rapidly as possible.