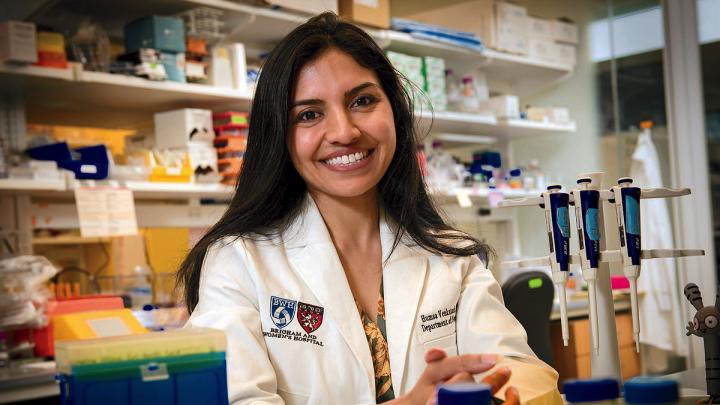
During the past two decades, the number of annual cancer deaths in the United States has fallen by 27 percent, a remarkable improvement driven by new precision diagnoses and treatments tailored to individual patients. Today, oncologists can detect cancer in its earliest stages and deliver drugs that enlist the patient’s own immune system to improve their odds of survival. Yet cancer remains the second deadliest disease in the United States, claiming more than 600,000 lives every year. Its persistence underscores the urgent need for a deeper understanding of how cancer interacts with the body. Assistant professor of neurology Humsa Venkatesh believes she may have found a promising new pathway for highly effective cancer treatments in the most unexpected of places: the human brain.
Venkatesh and her colleagues have been pioneering a new approach to oncology that she calls “cancer neuroscience,” focused on understanding the bidirectional relationship between cancer and the brain. Although researchers first observed that nerves are numerous around cancer tumors nearly a century ago, Venkatesh says this link was “largely ignored” as oncologists focused instead on the molecular and genetic features of cancer that could be targeted with precision drugs.
“Cancer biologists and neuroscientists were just in completely different worlds and never really crossed paths,” she says. “But over the past few decades, science has become extraordinarily interdisciplinary as communication and technology barriers began to fall.”
While pursuing a Ph.D. in cancer biology from Stanford, Venkatesh launched a series of experiments that applied neuroscientific tools and techniques to brain tumors for the first time. It was a high-risk gamble for an early career scientist entering a field that was largely focused on personalized cancer treatments, but what she found out about the link between cancer and the nervous system launched a new field of cancer research.
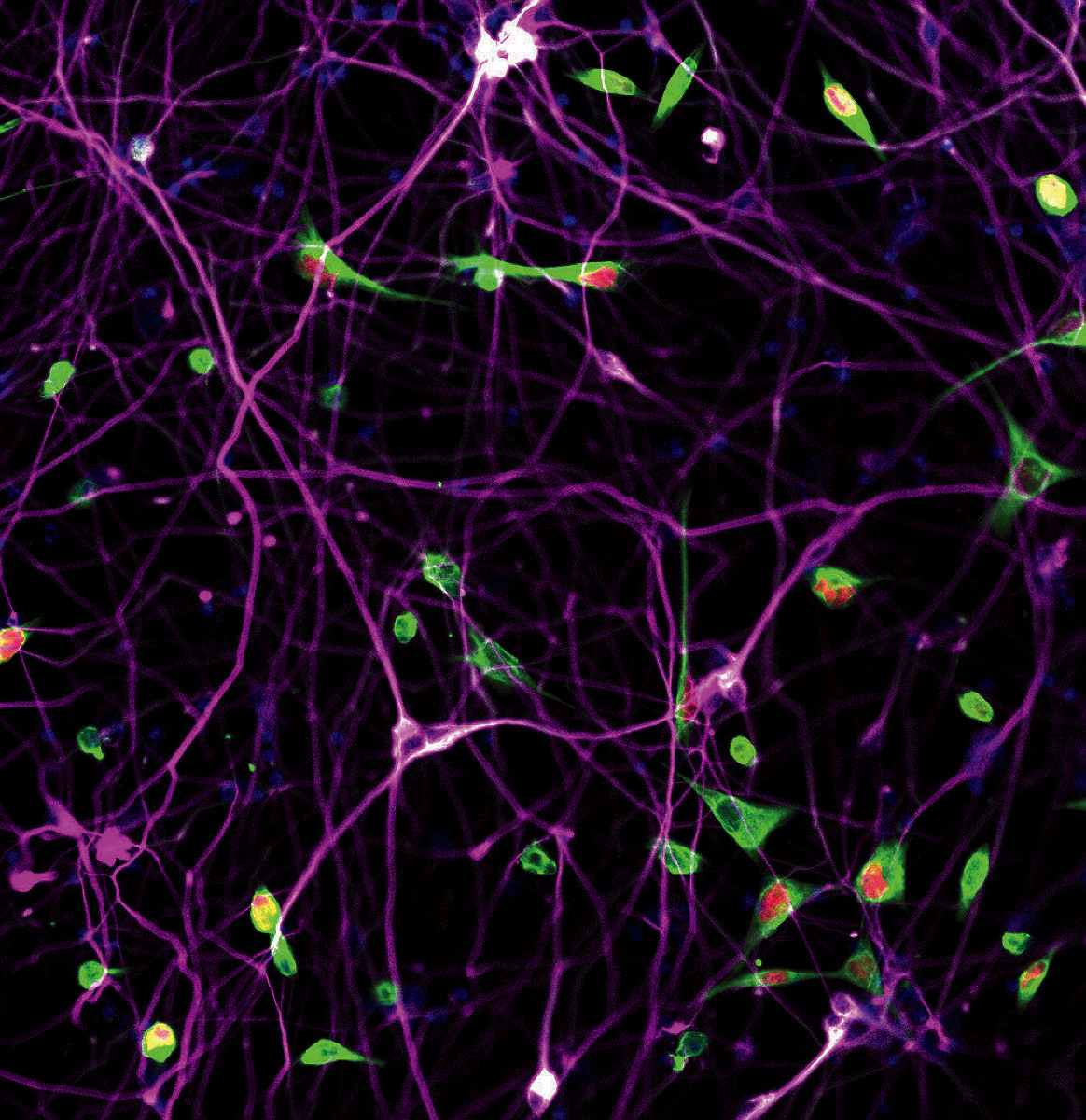
About a decade ago, she and her collaborators sought to determine whether increased neural activity promotes or inhibits the growth of gliomas, a type of cancer that originates in the brain. They used optogenetics—a method for precisely stimulating neural circuits using light and genetic engineering—to activate brain regions around a glioma and found that increased neural activity resulted in robust growth of brain tumors. “It was really the first evidence ever that neural activity can drive tumor growth, and we were really excited by those results,” Venkatesh said. “The next big question was, why does this occur?”
To resolve this mystery, she needed to think like a detective, using neuroscience tools to “wiretap” the communication channels between neurons and cancer cells to eavesdrop on their cryptic communications. After a few years of detailed observation, she had her answer. The heightened neural activity Venkatesh had induced in previous experiments caused the brain to produce a protein called neuroligin-3. When this protein interacted with glioma cells, it stimulated cell division, causing the tumor to grow.
This alone wasn’t particularly surprising. Proteins that stimulate cell growth are known as mitogens, and researchers have identified hundreds that play a role in tumor growth. But given the strong link between heightened neural activity and tumor growth, it didn’t seem far-fetched that this particular mitogen—neuroligin-3—might be the linchpin driving glioma growth. If true, reducing the amount of neuroligin-3 produced in the brain might stop the growth of the tumor altogether. When Venkatesh and her colleagues tested this theory in mice genetically modified not to produce neuroligin-3, “We found that the lack of this single protein completely abrogates the tumor’s ability to grow,” she said. “For those of us who work in cancer research, that’s really, really astounding. We know there are several mitogens at play that promote tumor growth, so if we take one away, we might expect some growth inhibition, but not something this stark.”
As Venkatesh dug deeper into neuroligin-3’s role in the brain, she realized that, beyond its known role of stimulating cell growth, this protein also helps neurons communicate. When it interacts with a cancer cell, neuroligin-3 enables that cell to communicate with other neurons as if it were a healthy cell. Even more surprising was the discovery that this communication was bidirectional: increased neural activity led to faster tumor growth, and faster tumor growth caused more electrical activity in healthy neurons.
“These tumors are essentially hijacking our normal brain mechanisms for abnormal neuroplasticity,” said Venkatesh. “This was the first time we had seen these bursts of electrical activity in malignant tumor tissue.This was a characteristic of tumor pathophysiology we had been missing.”
How to translate these exciting results in mice into a clinical treatment wasn’t obvious. Although several drugs—including antiepileptics and antidepressants—change the way neurons communicate, they target the entire nervous system and may have significant “off-target” effects. To treat gliomas, Venkatesh wanted a drug that would specifically target cancer by reducing the production of neuroligin-3. After a long search, she and her colleagues found one that appeared perfect for the job; it is being tested in a Phase I clinical trial in children with recurrent aggressive brain cancers.
“We’ve tested it in preclinical models in the lab, and we seem to have some really positive results,” Venkatesh said. “I don’t think that it’s going to be a silver bullet, but I think it could perhaps ameliorate the effects by lessening the overall amount of neuroligin-3 in the brain.”
As the researchers wait for the clinical trial’s results next summer, they’re exploring whether their results can be generalized to cancers outside the brain. Their first target is small-cell lung cancers, the most aggressive form of the deadliest type of cancer. It’s a natural next step, given that these malignancies tend to arise from “pulmonary neuroendocrine cells,” which have many features similar to neurons. This may explain why small-cell lung cancers have very high odds of metastasizing to the brain—a longstanding mystery in oncology—and makes them a promising starting place for understanding how neural activity affects cancers elsewhere in the body.
Venkatesh says it’s too early to tell how widely her results will translate to other tumors outside the brain, but the growing body of evidence she and her colleagues have accumulated has made her optimistic that cancer neuroscience will have an important role to play in developing new therapies that could save the lives of countless patients. Cancer researchers are, by nature, cautious of hyping novel therapies given the field’s long history of would-be cures falling short of their promise. Cancers, like the brain, are remarkably complex and no single approach is likely to rid the world of these deadly diseases. But after a decade of breakthrough after breakthrough, Venkatesh seems hardly able to contain her excitement about the future of cancer neuroscience. “The more I think about it, the more I appreciate how wild it is that we hadn’t gone down this path yet,” she says. “The field has been gaining so much momentum, and that’s just so exciting to see as one of the people who was lucky enough to be a pioneer in this space.”