The doctor asked the man to tell her what he remembered, and so he took a breath and began to speak. In the months since he’d left the intensive-care unit where he nearly died, he had been over these events again and again, searching his own memory and the recollections of his wife and daughter, trying to make the puzzle pieces fit. They never quite did.
But today was a different kind of exercise. The doctor, Daniela Lamas ’03, is a pulmonary and critical-care physician at Brigham and Women’s Hospital, where James (though that’s not really his name) had been transferred from another hospital when his condition went from bad to worse. After he’d returned home and settled back into daily life, Lamas reached out to ask if he’d be interested in a follow-up appointment, part of a still-evolving clinic she helped start four years ago, for former patients of the Brigham’s ICU. The idea is to see how these patients are faring in the aftermath of critical illness, to identify needs or difficulties, to talk about quality-of-life goals, and to answer any questions they might have about what happened to them in the hospital—because often, like James, they don’t fully remember. (“Why do I have this small hole here?” a woman once asked Lamas, pointing to the spot where a chest tube had been inserted and later removed.)
Occasionally patients request tours of the ICU, to see, with a clearer head, the place where they may have spent weeks or months. After each clinic appointment, Lamas types up detailed notes and recommendations to share with the patient’s primary-care doctors and makes referrals to other specialists as needed—social workers, often, or mental-health counselors. “We know that after the ICU, people suffer issues they didn’t have before,” she says. Some experience depression or anxiety or lingering delirium; as many as one-third have post-traumatic stress disorder. Others go home with cognitive changes—minds slowed by the medicines they took or the ordeals they endured. Until recently, ICU physicians have known little about any of this. After patients leave their care, Lamas says, “we don’t see them.”

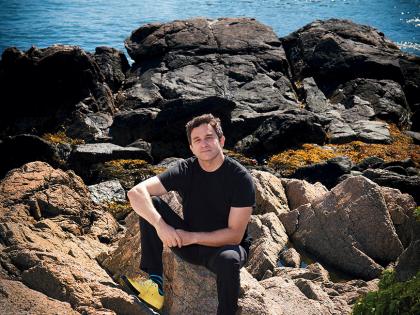
Daniela Lamas
Photograph by Stu Rosner
Making sure those patients are seen—in every sense of the word—has become a driving passion for Lamas. She is also a researcher in the serious-illness program at Ariadne Labs, a joint project of Harvard and Brigham and Women’s, started by Brigham surgeon Atul Gawande. And she is a medical journalist who writes for The New York Times and The Atlantic and published her first book last spring: You Can Stop Humming Now: A Doctor’s Stories of Life, Death, and In Between. It is a memoir of a decade’s work in intensive-care units, but also an immersive exploration of what patients’ lives are like afterward.
“She’s mining a space we haven’t opened up very effectively,” says Gawande, Thier professor of surgery at Harvard Medical School and of health policy and management at the Harvard T.H. Chan School of Public Health. “What Daniela’s ended up really recognizing is that six million people go into intensive care, and five million people are later discharged home. And what it is to return home after often incredible trauma and devastating illness, sometimes lingering difficulties and conditions—we haven’t explained or begun to uncover what that bridge is like, or what the gaps and challenges are. We’re helping people survive who never survived before, and it’s their struggles she’s given voice to.”
In a 2013 essay in The Atlantic, Lamas wrote: “As more adults survive intensive care, we’ve inadvertently created a new world populated by the walking wounded....I’ve come to fear that our best interventions are less meaningful, and our counsel to families shallow, if we don’t fully understand what happens to our patients after they leave our units’ doors.”
After the ICU
And so, at two o’clock on a November afternoon, Lamas and James, who is in his sixties, sat down for their appointment. They spoke by video conference call, an arrangement that saved him a journey to the hospital. He was at his desk at home, wrapped in a blanket; Lamas was at the Brigham, squeezed into a tiny office with three colleagues: critical-care physician (and post-ICU clinic co-founder) Gerald Weinstein, social worker Stacey Salomon, and psychiatrist Nomi Levi-Carrick.
James and Lamas traded narratives about his time in the ICU. Her version, taken from hospital records (she was not one of the doctors who treated him), went like this: he was first hospitalized in early summer, after feeling weak and falling down at home. The doctors at his local hospital soon realized he was very sick—his blood pressure was dropping and his kidneys malfunctioning, indicating that his body was in shock, likely from an infection. He was transferred to another hospital and then a few days later to the Brigham, where doctors discovered an area in his intestines that had burst open, and operated to repair it. They also found a clot in one lung and administered blood thinners. There were blockages in the passageways from his kidneys to his bladder, which were still being addressed. After several days in the ICU and two weeks on the hospital’s regular floor, James was released to a rehab facility. The breathing tube his doctors had inserted was removed. His health improved, and he went home.
James’s version of the story was more fragmentary, and much more frightening. He remembered the breathing tube; in fact, he said, “I was absolutely certain I had pulled it out.” (He hadn’t, Lamas assured him, though the sense of having done so is common and entirely normal.) He remembered hearing—or perhaps hallucinating—strange noises outside his room, “and I just knew I had to get out of there.” He also recalled wild, awful dreams that seemed as vividly real as any experience he’d ever had, about being taken against his will to different parts of the hospital, about being told by medical staff that his behavior was erratic and they were worried, about being stranded alone in a strange wing of the building.
“These are all things that make sense, even though they seem like they don’t,” Lamas said, reassuring him again. “Your mind was trying to make sense of your situation.”
The fear set in once James arrived home and realized how close he had come to dying. Pain and sleeplessness set in, too. His kidneys were still being drained by tubes attached through his back, which were uncomfortable and sometimes excruciating. He longed for the tennis court, where he and his wife had been a doubles team, and for the pub where he used to go for a pint and some conversation. Both were off-limits for now, and he was stuck at home for most of the day, alone, waiting for his wife to come back from work or his grandchildren to come over to visit. He cooked dinner and cleaned up around the house. He watched TV. When it wasn’t too cold out, he took short walks. “I’m OK; it’s nothing I can’t live with,” he kept saying—of the pain, of the broken sleep, of the isolation, of the fragility and fear. “I’m OK. It’s OK.”
But 20 minutes into the conversation, he paused. “You know,” he said, “sometimes the feeling I get is, what am I doing here? I’m sick of just sitting here sometimes. And I do get depressed....The big positive for me is that I’m still alive, and I’d rather be alive than dead. But once you get past that, I mean—what am I doing?”
His voice trailed off, and then Lamas spoke. “Everything you’ve told us,” she said, “it all gets to the issues we wanted to talk to you about.” She thanked him for his openness. “These are entirely normal things to deal with after what you’ve been through.” She was speaking slowly, choosing words carefully. “Thank you,” he said. He’d have a follow-up appointment with Levy-Carrick and Salomon. Lamas would speak to his regular doctor about the pain and sleep and other issues: “I’m really very hopeful that we can help you.”
The Walking Wounded
The pages of You Can Stop Humming Now are full of people like James. Lamas devotes one chapter to an artist who narrowly survived a tear in her aorta—the surgery involved an incision that wrapped around her torso from her navel to her upper back. She left the hospital harrowed by nightmares and post-traumatic stress. Her artwork, and years of therapy, helped her re-enter life.
But the book, and Lamas’s post-ICU clinic, also address another kind of “walking wounded”: the chronically critically ill, who, even after they leave the ICU, remain caught in an overwhelming orbit of sickness and care. Lamas writes about a man whose bout with West Nile virus nearly killed him; after several weeks in intensive care, he emerged tethered to a ventilator, a feeding tube, and a urine catheter. She writes about a grandfather with heart failure who stays alive, and relatively active, with the help of an implanted mechanical heart pump. Every night he must plug the device into the wall and wait “like a dog on a leash” for its batteries to charge, and, a fisherman, he can no longer ride in a boat—falling into the water would electrocute him—but he can still fish from the shore with his grandson. Lamas spends time with a 30-something cystic-fibrosis patient living through an adulthood she never expected to reach, and with a young mother who receives a lung transplant just in time to save her life, but finds the road back to health long and bumpy—and scary and sad—in ways she didn’t foresee.
At any given time, Lamas writes, there are 100,000 chronically critically ill patients in the country, a population largely created by the breathtaking triumphs of the ICU, where doctors routinely save lives that even a few years ago would have been lost. But these seeming miracles also make possible long-term traumas, and life-saving interventions often turn out to be only the starting point for further interventions and quality-of-life concerns that are, Lamas says, far too little understood. “We’re talking a lot about the end of life these days,” she says, “but this sort of not-dead and not-alive moment of illness and recovery—that story is not as present.”
“The impact Daniela is having on the profession is profound,” says Bruce Levy, chief of pulmonary and critical care at the Brigham. “As physicians, we make decisions at a time of stress and crisis. And she’s opened windows to educate us on the downstream ramifications for patients.”
Not an Achievable Goal
Lamas’s interests were always split between medicine and writing. She was born at the Brigham—her father is former Harvard cardiologist Gervasio Lamas, who now practices in Miami. Medicine was always Lamas’s eventual destination, but she loved writing from childhood. She was a high-school-newspaper reporter and in college she joined The Harvard Crimson. “That was my world, that office,” she says. “I felt like I had a very important job.” One summer she interned at an alternative weekly newspaper in Miami, and the following summer, at The Miami Herald, which later hired her as a full-time reporter. She spent a year driving around the city in her Volkswagen Beetle, looking for stories.
After that, she went to medical school at Columbia. “I felt at first like I had made a devastating decision, leaving writing,” she says. Medical school felt like a strange version of college, where the only assignment was to memorize science, “and then when you were done memorizing, you were supposed to be really enthusiastic about playing beer pong.”
During residency, though, she fell in love with critical care. The patients in the ICU were the most compelling she saw, and she remembers watching the doctors there navigate decisions and communicate with families in moments of acute stress. “I wanted to be them.”
She also returned to writing. She took medical-reporting assignments for The Boston Globe and began writing in The Atlantic, The New Yorker, and The New York Times about her patients and her ICU experiences—thoughtful, affecting, humane essays on the profundities of her daily work: last wishes, home hospital care, the limbo between life and death. She wrote about smuggling a beer in to a dying patient and about spending Christmas in the ICU. A few years ago, when a literary agent urged her to write a book, she started seeking out stories from ICU survivors.
Her experience with those survivors has begun influencing Lamas’s work inside the ICU. She notes, for instance, that the ventilator is often a demarcation point for the critically ill, something patients and their families don’t always realize when they are crossing it. “I’ve become better at discussing the tracheostomy decision,” she says, referring to the surgical procedure that creates an opening in the neck that allows a breathing tube to be attached to the trachea. “Before, I really framed it as, ‘Now it’s time for a procedure to offer a more comfortable longer-term connection to the ventilator that will allow your loved one to get better.’ All of that is true, but it’s also true that once you have this thing, you’re probably not going to go home right away.” A more likely destination is a long-term-care facility, and recovery is often slow. “Even in the best-case scenario,” she says, “it’s really hard to get back to where you were—and maybe impossible.”
Her goal isn’t to change the decision, but to manage expectations. “We ask patients and their families to make decisions in acute, insane moments,” she says. And it can be tough in those moments to grasp the consequences, even if they’re spelled out. Still, Lamas says, “I think it’s important to set out the risk, so that people have some understanding of what gamble they’re making.”
Embedded in dilemmas like this one, and in the narratives in Lamas’s book, are ancient questions: what it means to save a life, or to live one; the connection between health and selfhood; and the murky boundaries of being “OK.” In the book, Lamas recalls a moment in the ICU when a patient’s worried daughter asked, “She’s going to be OK?” Lamas writes: “There it was. I had heard that question so many times, ending with that same word, OK. I had said the same thing to myself. In a way, it was an easy kind of shorthand. And yet I had rarely paused to ask a key question of my own response: What does it actually mean to be OK? The more I looked, the more complicated that answer had become.”
Her fellowship at the Brigham offered an early glimpse of the complications. She undertook a project interviewing patients at Spaulding Hospital in Cambridge, a long-term-care facility where people often land after the ICU. She had been studying end-of-life conversations and wondered about the possibility of an adjacent discussion, on goals and values and health expectations of patients with critical illness. She spent weeks at Spaulding, interviewing patients who were on ventilators. What she learned, she says, was dispiriting but not surprising: their expectations for their future health were largely unrealistic, and their quality of life was often terrible. They were enduring in the hope that they would eventually go home and resume functional, independent lives. “Which for many of them is not an achievable goal.”
Those interviews stuck with her. Today at Ariadne Labs, she researches conversation tools to help doctors talk effectively with seriously ill patients about feasible goals and quality-of-life recommendations. “Usually people think about that as having a better death,” Gawande explains, “but it’s really about how you live as well as you possibly can in the face of impairment at the very end.”
Lamas had one of those conversations a few months ago, with a patient who came to the Brigham for a lung-transplant evaluation. As it became clear that his chances were dim—other health problems made the surgery dangerous—Lamas began nudging him and his family to imagine a life without new lungs. What did “OK” mean to him? Medical interventions could lengthen the time he had left, but would mean more trips to the hospital; forgoing those treatments would allow more comfort at home, but his life would likely be shorter. “It’s easy to come in with a set idea of what a ‘good’ process through the medical system looks like,” she said later. “But what’s tolerable can be very different from one person to another—talking to ICU survivors has taught me that. If anything, their stories have made me more open-minded about what is OK.”