In a world that prizes medical science and blames illness on factors such as genes, viruses, bacteria, or poor diet, certain perplexing cases stand out. Consider babies in orphanages who have had all their physical needs met, yet fail to develop because they lack a strong connection to another person. Or the roughly 200 women in Cambodia with perfectly healthy eyes who became blind after they were forced to watch as loved ones were tortured and killed. Or Mr. Wright, a man whose tumors “melted like snowballs on a hot stove” when he was given Krebiozen, an experimental drug that he believed would cure his cancer, but was later declared to be worthless by the American Medical Association.
These cases underscore the powerful idea that the mind matters in sickness and health. Judging by the millions of Americans who use mind-body modalities such as yoga, meditation, qi gong, and massage to fight diseases like cancer, it’s an idea that many accept.
But why do we believe in the mind-body link in the first place? Anne Harrington, professor of the history of science and chair of the department, says we’re only partially convinced by laboratory studies revealing which of these therapies do and don’t work. “Science is only part of what has created mind-body medicine and sustains it today,” she notes. In her recent history, The Cure Within, she argues that we’re also persuaded by stories, especially a key set of narratives that humans have told about the mind and body through history. These stories, she says, help us make sense of complicated experiences like illness and suffering.
For example, the cultural power of some mind-body ideas becomes clear when you trace them back to their roots in religion. Groups such as the Christian Scientists drew from the New Testament the message that strong faith can yield miracle cures, and Harrington shows how this led eventually to self-help bestsellers about the therapeutic effects of positive thinking.
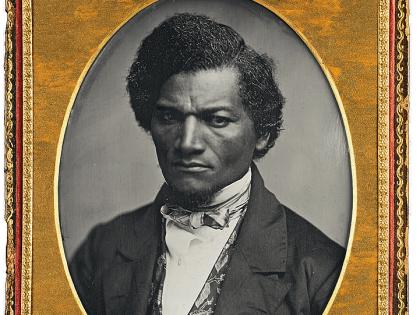
In the secular arena, she continues, post-World War II anxieties produced stories about the ways our minds leave us vulnerable to illness, including “the idea that we live in a world that we weren’t made to endure, that taxes our energies beyond our capacity.” At the center of that narrative she places physical and emotional stress, a relatively new concept that was formulated near the end of the 1940s by the Czech biochemist Hans Selye, who borrowed the term from metallurgy. The concept subsequently gained traction as psychiatrists studied traumatized soldiers and, later, overworked executives, especially those with Type A personalities (thought to be prone to heart attacks). During the decades since then, Harrington says that concern about stress and the illnesses it may trigger have escalated.
But these laments centered on modern life have also yielded some hopeful mind-body stories: “efforts to narrate our way out of the darkness,” in Harrington’s words. For instance, one type of narrative maintains that we can stay healthy or even heal ourselves through strong relationships. Another set of stories finds promise in the healing practices of Eastern cultures, an interest that burgeoned with the Beatles’ trip to India to seek the spiritual guidance of the Maharishi Mahesh Yogi; was sustained by the late 1970s discovery—by Mind/Body Medical Institute associate professor of medicine Herbert Benson—of the meditation-derived “relaxation response” to counter stress; and continues to be the subject of Harvard research: for example, scientists are studying MRI scans of the brains of meditating Tibetan monks.
Harrington says that it’s useful to consider when we find these mind-body stories most convincing. “It’s often when we’re let down by the mainstream medical narrative of Western society”—which values concrete solutions and statistics. Such an approach fails to help chronically ill patients grapple with questions like “Why did this happen to me?” Mainstream medicine, Harrington continues, “often will answer that there is no reason, or that in effect the reason is dumb bad luck. Mind-body medicine is a tempting alternative for patients in such moments because it is all about connecting the ‘why, when, and what now’ of an illness back to a person’s biography.” Mind-body narratives give us a vocabulary for complex experiences like discontent and hope, she adds. “Stories can do things that science can’t.”