In the United States and globally, the inability to test large numbers of people for COVID-19 has severely hampered diagnosis by clinicians and the data-gathering and modeling efforts of epidemiologists. But the shortage does not involve testing capacity, experts say: analytical laboratories could handle far more tests than they currently process. The bottleneck lies in supplies: specifically, says assistant professor of epidemiology Michael Mina, “a 26-cent swab.”
Globally, nasopharyngeal swabs have been in short supply since March. Nothing else can be inserted far enough into the nose as effectively to sample mucus in the nasopharynx, where a tiny passage connects the nose to the top of the throat. “Experts have recently estimated that the United States needs to more than triple the number of daily COVID-19 tests in order for the country to be safely reopened by mid May, says Richard Novak, Ph.D., a senior staff engineer at the Wyss Institute for Biologically Inspired Engineering at Harvard, who has been leading a multi-institutional effort to develop a simpler swab. “But the current swabs are complicated to make, and producers just don’t have the ability to increase production to that level in such a short period of time.”

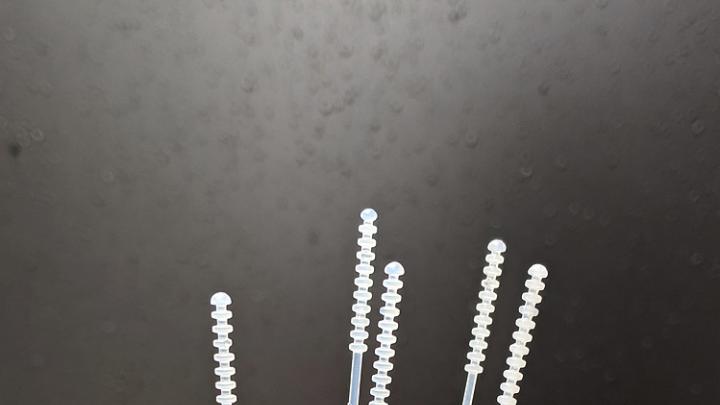
Richard Novak designed a swab that can be produced using injection molding.
Photograph courtesy of the Wyss Institute at Harvard University
The swabs used to collect samples in the United States have long been manufactured principally in Northern Italy and in China, where COVID-19 hit early and hard, crippling production. Furthermore, the swabs were not considered an essential item for the U.S. national strategic stockpile. As the extent of this supply problem emerged, assistant professor of pathology Ramy Arnaout, the associate director of the clinical microbiology laboratories at Beth Israel Deaconess Medical Center, turned to the scientific community for help.
In the ensuing brainstorming, the idea of producing the swabs using 3-D printing proved the best short-term solution, and several prototypes were developed. By April 9, an ad hoc consortium organized and led by Tarr Family professor of bioengineering and applied physics Kit Parker and Ric Fulop, CEO of the 3-D printing company Desktop Metals, had announced that swabs of their design could be ordered from several different manufacturers in the United States. But 3-D printed swabs are expensive to manufacture—and the facilities to mass-produce them don’t exist in Europe, India, China, and Africa says the Wyss Institute’s founding director, Donald Ingber, Folkman professor of vascular biology and professor of bioengineering.
He and Novak, who has an extensive background in plastics manufacturing, focused instead on designing a swab that could be mass-produced globally—and at low cost. The challenge, Novak explained in an interview, is that “the swab must be very thin, and has to have just the right amount of flexibility.” The swabs are inserted through the nose to a point “almost between your ears. They go really far in, through the nasal turbinates to the spot where your throat meets your nose, at the base of the brain. There is the potential to do damage because this area is very fragile.”
At Ingber’s request, the 3M Company sent him a box of dozens of different sample swabs they manufacture for other purposes, to see if any might be repurposed. But the anatomy of the human skull, combined with the fact that the highest load of virus is located deep inside it, meant that only a specialized swab would work. According to a statement from the Wyss, “The nasopharyngeal swabs that have been used in hospitals for over 50 years consist of two pieces: an injection-molded plastic handle and an absorptive tip made of a soft material such as cotton, polyester, or flocked nylon. Each swab is manufactured in a multi-step process, then assembled, sterilized, and packaged, all of which requires significant time and expense.”
Novak and colleagues on the Wyss’s advanced-technology team therefore decided to design a swab that could be manufactured as a single piece using injection molding. In this process, hot plastic is forced into a mold designed with cavities for perhaps 50 or more swabs, and each manufacturing cycle takes fewer than 10 seconds, explained Novak. Injection molding is fast, inexpensive, and is already used by medical-device manufacturers worldwide. Prototypes of the design—with a tip shaped like the evenly spaced stacked discs on the familiar dippers used for honey—are being tested in hospitals nationwide this week. If these human trials prove successful, California-based medical-device manufacturer IPB, Inc. is prepared to produce 200,000 swabs per day by May 15, at a cost one-third to one-fifth that of 3-D printed swabs.
Novak notes that the design is open-source; there are no intellectual property claims or licensing restrictions. “In this sort of situation,” adds Ingber, “agility and a can-do spirit really come to the fore. I’m proud of Richard and his team… because I think this is something that could translate internationally. We may need to optimize the design when we get the clinical results back, but the fact that we got this to a point that, if it works, it can be scaled up to enormous proportions, is very important.”