Khaled became my patient 41 years ago, when he was a tiny misshapen six-year-old with paper-thin, distorted bones. He was close to heart failure and so anemic when I met him that his blood was watery. I thought he might die in front of me.
He has thalassemia, a severe anemia arising from the inheritance of two defective hemoglobin-production genes, one from each parent, both of whom are healthy (albeit mildly anemic) because they each carry only one such defective gene.
There are many thousands of patients like Khaled throughout the old malarious world, but only a handful in the United States. The many ancient gene mutations that shut down hemoglobin production in red blood cells have been preserved and enhanced in humans because infant carriers of the mutations are partially protected from a particularly lethal type of malaria. Therefore the thalassemia genes have persisted by Darwinian natural selection of carriers; an unfortunate circumstance in which a disease gene persists because it provides partial protection from a lethal infection. The result is the proliferation of carriers and the birth of thousands of babies with two defective genes who become profoundly anemic and require lifelong transfusion of red cells. The patients--the “lucky” ones--are huge consumers of medical care; most often, the carrier parents face the loss of their child at an early age.
During the past four decades I have been forced to give Khaled red-blood-cell transfusions every three to four weeks. Such treatment, though an absolute requirement of his care, is fraught with devastating complications. Consequently he has had to endure and surmount one massive medical assault after another. But he has survived, and today he is a successful entrepreneur. Nonetheless, he has been battered by all the major consequences of managing his disease. His success is largely due to his own resilient, positive outlook (admittedly maddening when he would refuse to do what I told him to do), the support of his family, the commitment of Children’s Hospital Boston and its entire staff to children in need, and the continued and remarkable explosion in biomedical and pharmaceutical science that permits physicians like me to offer care that was impossible when Khaled and I first met. In this 40-year relationship--fully half my own life--I have found unexpected lessons about doctoring, the advance of medicine, and our system of healthcare itself.

Courtesy of Deborah Chirnomas, M.D.
Thalassemia patients need regular transfusions of red blood cells, but the therapy eventually causes death by overloading the body with iron. These MRI cross-sections show a patient’s heart (upper center) before and after treatment: in the image at right, the septum (the wall dividing the heart) is full of iron, which also darkens the liver and spleen, below the heart. Recently, chelator drugs have been developed to eliminate iron from the body.
The first 25 years of Khaled’s journey were immensely frustrating. We were learning a lot about his disease, but not enough to give him the quality of life that we wanted for him. We have made much more progress in the past 15 years. Drugs and imaging systems have been developed that allow physicians far more capacity to manage or prevent the lethal consequences of chronic red-cell transfusion (see below). Many patients with thalassemia have been cured by bone-marrow stem-cell transplantation. Gene therapy, thought to be impossible only a few years ago, has become a viable option for some rare, inherited blood diseases (though thalassemia is not yet one of them).
As a result of this progress my patient and I this spring were able to jointly celebrate his forty-seventh birthday and, parenthetically, my eightieth. Four decades ago, when I was a brash 40-year-old physician, I pledged to his parents that I would not rest until he was on a course that would permit him to outlive me. In retrospect, that promise was the product of hubris or suicidal ideation. Any experienced hematologist would have expected him to die before the age of 20. But biomedical science and clinical research intervened, and here he is.
Much of the saga of those first 25 years revolved around the most pernicious hazard of chronic red-blood-cell transfusion--iron overload. Every ounce of red blood cells contains 30 milligrams of iron. One year of monthly transfusions of a pint of red blood cells will push 5 grams of iron into the body, more than the total amount of iron in a normal adult. The body has no way of eliminating iron forced into it from the outside. Prior to the advent of drugs called chelators that grab iron and eliminate it from the body through the kidneys and the gastrointestinal tract, almost all children dependent on red-blood-cell transfusions died of iron-induced heart failure before the age of 20.
My efforts to persuade Khaled to self-administer deferoxamine, the first available iron chelator, were entirely frustrating. That drug cannot be taken by mouth; it must be administered by a portable pump attached to a syringe and needle that slowly pushes the drug under the skin for at least 10 hours a day, five days a week. Though deferoxamine is life-saving, almost half the patients with thalassemia cannot bear the routine. Khaled particularly hated it because the procedure produced painful welts.
His failure to do as I asked (called non-compliance by the cognoscenti) induced at least five episodes of heart failure, from which he was rescued only by hospitalizing him, placing a plastic tube in one of his veins, infusing deferoxamine around the clock for three weeks, and then discharging him to continue the treatment by using the pump attached to the catheter. One such tube lasted in one of his arm veins from 1988 to 1995. In that period we infused deferoxamine into him 24 hours a day, seven days a week while he went about his daily life and saw us every three weeks for transfusions. His heart function greatly improved, but the miraculous vein eventually collapsed and we were left with the same problem--how to achieve a sufficient dose of deferoxamine.
Had iron overload been his only problem, Khaled’s medical care might have been less complex. Sadly, my patient contracted both HIV and hepatitis C from infected blood, as did so many regularly transfused patients in the 1980s, when much of the nation’s blood supply was contaminated. (Ironically, he received his transfusions at that time at the National Institutes of Health, which has one of the best, if not the best, blood banks in the United States.) The mid 1980s was a terrible period in transfusion medicine. Thousands of recipients of red blood cells or plasma products became infected. The isolation of those viruses and the development of reliable screening tests saved the world’s blood supply, but the unfortunate patients who received contaminated blood products before the screening tests became available were terribly damaged, and many have died.
Fortunately for Khaled and many patients like him, the pharmaceutical industry has ridden to the rescue. Transfusion-induced HIV infection can be controlled with three or four different antiviral agents. The virus cannot be eradicated, but full-blown AIDS can be avoided and the patients can live normal lives--albeit with drug toxicity of variable severity. Since the introduction of drugs called protease inhibitors, for example, the death rate from AIDS in the United States has declined precipitously--but one of its most difficult side effects is a redistribution of body fat, together with wasting of the muscles. Khaled has dealt with that complication as best he can.
In 2006, we became concerned that his long-standing hepatitis C virus infection was beginning to damage his liver. Fortunately, pharmaceutical companies and clinical investigators had come up with a combination of drugs and an antiviral protein called interferon. The combination is known to eradicate hepatitis C in almost half of the infected patients who were otherwise normal. There was much less experience of this treatment in multiply transfused patients with severe iron overload. We should not have worried. Though Khaled endured several debilitating complications of the treatment, one of which forced us to give him even more iron-laden red-cell transfusions, the virus was eradicated and he is free of the infection today.
The major threat to his life was and remains his borderline heart function. Several bouts of acute iron-induced heart failure with fluid accumulation, weakness, and shortness of breath have left his heart muscle cells permanently damaged. These specialized cells divide at an extremely low rate; in effect, the heart muscle cells with which one is born are largely those with which one dies--so progressive damage to heart muscle cells inexorably leads to heart failure. That was why we were desperate to find a way to provide Khaled with a sufficient amount of an iron chelator. We knew that his heart would not tolerate more muscle loss from iron overload.
In 2001, his heart failure suddenly worsened, not because his iron load had exploded, but because his heart rate had increased markedly and the beat was irregular, a condition known as auricular or atrial fibrillation. The iron toxicity seemed to have spread to the nerves that conduct the electrical signal from the low-pressure heart chambers called auricles to the high-pressure chambers called ventricles. That signal controls the heart rate. The signal gathers steam in the auricles and stimulates them to contract, passes to a special switch box between the auricles and the ventricles, and then spreads into the ventricles to tell them to contract. Khaled had an injured place in his auricles that was making the signal run wild in those low-pressure chambers. They were quivering but not beating. The ventricles were receiving multiple high-speed messages from the auricles and beating much too fast. The high pulse rate prevented them from filling adequately. That problem, together with the ventricle muscle damage, was causing heart failure.
We did everything we could to correct the atrial fibrillation with drugs and with electrical stimulation of the heart delivered by external electrodes. None of our efforts could hold him in what is called normal sinus rhythm for more than a few days, or sometimes weeks. Finally we decided to send Khaled to Bordeaux, France, where a new approach to the treatment of such rhythm disturbances had been developed. A cardiac catheter was placed in the auricle, the injured site located, and the site burned out with a jolt of electricity. It worked! Khaled has had a normal heart rate ever since. That method is now used widely around the world, and we can do it very easily in Boston. Medicine is an international venture.
In addition to his battle with HIV, hepatitis C, and auricular fibrillation, Khaled had to contend with another serious complication now observed in surviving thalassemic patients--severe loss of calcium from bones, the cause of which is not exactly clear. He had had many fractures in early childhood because his bone marrow had expanded so much that it had weakened the structural component of the bones themselves. After we transfused him and raised his hemoglobin, his bone-marrow volume receded and x-rays seemed to indicate that his bones had improved markedly. But his marrow volume was still higher than normal and over the years, special scans of his bones revealed that their calcium content had again declined. The loss was particularly severe in his ankles and feet. He needed supplementary calcium and vitamin D. These worked for him: bone pain in his ankles and feet has diminished.
Still, the most pernicious and dangerous problem remained iron overload. In 1995, when it became impossible to maintain him on deferoxamine by constant intravenous infusion, we were forced to return to the much-hated, pump-assisted constant injections under the skin. Khaled knew that his life was at stake. He was then 33 years old and had a lot to live for. He had a highly supportive family, some very promising if difficult business opportunities, many friends, and an optimistic view of life. He decided to cooperate with the treatment plan, even though he loathed it.
Our job was to try to find a better chelating drug--one that he could take by mouth along with his myriad of other medications. For the next seven years we struggled. There was one orally active drug then available in Europe that was undergoing what became a highly controversial trial in Canada. The Canadian investigator allowed me to try the drug, but Khaled had an immediate toxic reaction with terrible arthritis and hepatitis. Massive amounts of iron leaked out of his liver. It was clear that the controversial drug was not for him.
Then, in 2002, we had a fortunate break. Ciba-Geigy, the only major pharmaceutical company with an interest in iron chelators, and Sandoz Pharmaceuticals combined to form a new and much larger company, Novartis. The iron group at Ciba-Geigy was truncated, but still active. They did not have the resources to screen natural substances for iron-chelation capacity, but they could screen the world’s literature and look for descriptions of promising compounds that their medicinal chemists could tweak and make into a useful orally active chelator. They found such a compound in an obscure Russian chemical journal, pounced on it, and made it into a drug they called ICL670. Later it received the generic name deferisirox and a trade name, Exjade. After suitable animal-toxicity studies, they gave ICL670 to me and my colleagues from Canada and the Weill Cornell Medical School to carry out what is called a phase 1 trial in patients with thalassemia.
To determine whether the drug was effective was no easy task because, unlike deferoxamine, ICL670 does not remove any of the iron it captures through the kidneys. A simple analysis of urine iron content was therefore useless. We had to put the patients into special research beds and collect all their stools, day after day, for two weeks as they swallowed doses of the drug. When the stools were measured for their iron content, it was clear that the drug worked and that, in the relatively short trial, it was not toxic. We published the results in 2003.
Novartis immediately set about to run a complex so-called phase 3 trial in which they compared the new orally active ICL670 with deferoxamine pumped under the skin. To do so, they used highly complex and nearly unavailable machines that measure iron in the liver. The results were promising. In that longer trial the drug was as effective as deferoxamine and toxicity was not a serious problem.
Novartis is a very careful pharmaceutical company, and the process of drug approval in the United States, and to a lesser extent in Europe, is terribly difficult and expensive. Most drugs fail to win approval, or turn out to be useless, even after hundreds of millions of dollars are spent on the animal and clinical trials performed to evaluate them. The last thing Novartis officials wanted was to treat a patient like Khaled, whose brittle condition might lead to a poor outcome whether the drug was to blame or not. But they agreed to establish a special clinical trial for patients like him, and in the summer of 2003 he was started on deferisirox.
That was a huge turning point. He tolerated the drug well, and we were soon able to measure its effects on his iron stores because experts in the imaging sciences in England and Australia had developed special programs for standard magnetic resonance imaging machines that permitted assessment of the iron content of the liver and the heart. Gone were the hugely expensive, generally unavailable machines previously used to measure iron (and even then, only in the liver). Now we could see whether the drug would work for Khaled. We took him off the hated deferoxamine and its infusion pump and watched his heart function and his heart and liver iron as he took a daily oral dose of deferisirox. The results were excellent. We had to increase his dose to get the blood level of drug that we needed, but his heart remained stable despite the lack of pumped-in medicine. Deferisirox has performed well for the past six years, and Khaled’s body iron has slowly declined.
Are we out of trouble? Of course not. Transfusion of red cells every three weeks is neither desirable nor safe, and Khaled has been badly damaged by the procedure over the years. But he can now move about without that accursed pump and have an independent life. He travels extensively; he is very busy running a restaurant in his home city; he is constantly seeking new economic opportunities, while at the same time he devotes time and energy to the support of a camp for children with severe blood diseases and cancer. He remains a marvelous friend whom I visit when he comes for transfusions. We talk about his family, about the impossible behavior of the Israelis and the Palestinians, about the stupidity of the Bush administration, about Obama and the huge boost in morale that he has engendered, and about his own philosophy of life.
In a recent conversation he told me about some of his own reactions to the events of the past 15 years. I taped his remarks.
The turn of the century was a huge turning point for me. I lost everything that year: my telephone business, my girlfriend--everything. I was close to 40 and I really went through a tough patch. I wasn’t at all happy. Of course I had made money very fast in my twenties and I just didn’t have the wisdom or maturity to hold on to it. I was more focused on dying than living.
Now, in my forties, I have had to start all over again and I am glad because now I feel I have something to live for. I really believe that I will live, and I want to live to have simple pleasures like family and friends and helping kids in need. So now I am doing two kinds of business. I do a lot of consulting and arranging with Chinese construction companies, finding them projects in the Middle East. But there is plenty of downtime between deals, so I have gone into the restaurant business where I live. That’s a big success and it’s a service business--bringing pleasure to customers. I really like that.
I probably won’t have children of my own, but I have my wonderful nephews, whom I am close to and who bring me so much joy; I am so proud of them. I am also very proud of my involvement over the past 20 years with the Hole in the Wall Gang Camp, started by Paul Newman for kids with life-threatening diseases, some of which are far worse than mine. I was able to raise a $5-million gift for the camp from the Saudi government on behalf of the people of Saudi Arabia. That gave me a lot of satisfaction. I wish that camp had existed when I was a kid. It would have done me a lot of good. Twenty years after I raised that gift, we have over 50,000 children who have gone through the various camps--we have 12 of these camps now, all over the world.
When I was taking that interferon for hepatitis C, I was so sick that I thought I would die. My mother thought I was falling apart. She freaked out for the first time--not in front of me but with my brothers. They told me she thought I was dying. Maybe she was right--I had to drag myself to work. It was exhausting and my skin fell apart. I had a horrible rash. But I made it and I’m cured. Like so much of what I have been through--it was worth it. That new oral chelator is saving me. I’ve got a life now, and I’m going to keep it.
When I hear Khaled talk about himself in this unguarded way, it confirms my admiration for him. He started his life with a huge medical disadvantage. He would surely have died had it not been for the fierce devotion of his family, who applied their considerable resources to give him every opportunity to survive. But he had to have a strong will of his own to go through the assaults marshaled against him by his disease and our attempts to treat him. He has matured through it all. I get huge pleasure from his success.
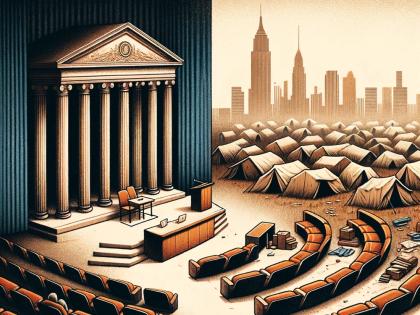
But at the same time, I worry about the future of the kind of medical care that we have provided Khaled. We have spent millions of dollars on his care alone. The scientific basis of that care would never have been developed were it not for a huge public investment in biomedical research (through the National Institutes of Health), the research budgets of other nations, private foundations, and the massive investments of the pharmaceutical industry. Had Khaled relied for his care on the fractured U.S. health system, he would have found himself penniless within a decade. Almost every private insurance company would have dropped him long ago. His staggering health costs were underwritten by a government because he is the son of a very highly regarded former diplomat and cabinet minister--scarcely a model that can be emulated.
When I try to visualize how we could find the resources to provide such treatment to an uninsured or underinsured U.S. citizen, I cringe. Yet I know that we have learned an enormous amount from Khaled, information that has been confirmed by others and then applied far more efficiently on behalf of other thalassemia patients in better-organized health systems around the world.
We are fortunate, here in the United States, that physicians like me, whose careers are devoted to clinical research in academic health centers, have the time and support to contribute to new treatments. But the application of those treatments to patients requires a cost-conscious and highly organized health system that is far from our ken in this country. I’m not sure that our citizens, our medical community, or our political leaders truly understand how broken the system really is. It must be reorganized if we are to provide this kind of research-based care to the many patients with serious chronic illnesses who need it, while we also offer high-level primary and preventive care to the vast population at large.
Meanwhile, I stay on the job, looking for patients like Khaled who can be helped by a creative union of physicians, nurses, basic scientists, and pharmaceutical companies. Those patients are the challenges who bring me to work every day. It’s an exciting honor and privilege to serve them.